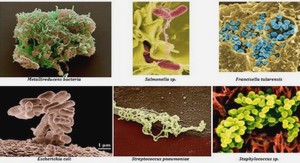
Attribution de source appliquée à Salmonella dans différents pays européens
Human salmonellosis is a major cause of disease in Europe. In 2006, the incidence of human salmonellosis in European Union Member States (MS) was 34.6 per 100,000 inhabitants (EFSA, 2007). A wide variability is observed amongst the countries, and incidence estimates ranged from 3.0 to 321.5 per 100,000 population in the different countries (EFSA, 2007). This variability also reflects differences in surveillance and reporting systems in European countries. During the last decades, several countries have implemented intervention programmes to prevent and control foodborne diseases, particularly foodborne zoonoses (Wegener et al., 2003; EFSA, 2006). However, precise measure of the public health impact of such interventions has been difficult, in part because the contribution of specific sources to the burden of foodborne diseases is often unknown. To prioritize appropriate food safety interventions, it is crucial to attribute the human disease burden of each foodborne infection to specific sources (Pires et al., 2009).. In order to get a better understanding of the mechanism behind the dynamics in the occurrence of Salmonella infections in humans, Hald et al (2004) developed a microbial subtyping approach for source attribution. The method estimates the number of human cases attributable to each of the major animal-food sources. The method is routinely applied by the Danish Zoonosis Centre, National Food Institute, and its results are published in the Annual Report on Zoonoses in Denmark (e.g. Anon., 2006). Microbial subtyping has proved to be a valuable tool in focusing food safety interventions to the appropriate animal reservoir in Denmark, and provides an example of potential synergy between quantitative risk assessment and public health surveillance (Wegener et al., 2003;Hald et al., 2004). An attempt to adapt the model to other European countries’ data was made under the scope of the “Human Illness Source Attribution” working group supported by Med Vet Net (WP 28). National source attribution models for Salmonella were developed for Germany, United Kingdom, the Netherlands, Sweden, Poland, and France. The method was adapted according to the availability and features of the data, and the interpretation of results took into account differences in public health processes, animal and food production, and food consumption figures. We present a comparison of the methods and results from these models and the model applied to Danish surveillance data.
Model overview
The model is built on the basis of the method described by Hald et al. (2004), where Salmonella subtypes isolated from animals and foods in a given year are compared with subtypes isolated from humans. The objective is to estimate the number of human cases that can be attributed to each source. The method is developed under a Bayesian framework and allows for the estimation of the contribution of additional factors, other than the prevalence of each type on the food/ source and the amount of food consumed, to the number of people infected with a particular type. These factors account for the differences in the ability of different Salmonella subtypes to cause disease and of different sources to act as a vehicle for infection. The basic model attribution equation is λji = Pij * mj * aj * qi (Equation 1), where λji is the expected number of cases per type i and source j, Pij is the prevalence of type i in source j, mj is the amount of source available for consumption in the country, aj is the source-dependent factor for source j, and qi is the bacteria dependent factor for type i. The source and subtype related factors aj and qi were defined as uniform prior distributions. qi for phage types within S. Enteritidis were fixed to 1, and all remaining qi estimates are relative to this one.
Data used in the model
The original model attributes human sporadic and domestic Salmonella infections to specific sources based on the number of laboratory-confirmed infections caused by each Salmonella subtype, travel information for each case, prevalence of each subtype in the different sources, and amount of source available for consumption in the country. The number of outbreak cases per type (except 1 case) is subtracted from the total number of cases 129 reported per type to estimate the number of sporadic cases. The remaining outbreak-related cases are in the end added to the output of the model. Travel information and amount of food source available for consumption are not an absolute data requirement, and the model can be adapted without these parameters. The variables and data differed between countries (Tables 1 and 2). This reflects differences in data availability with regards to typing of Salmonella isolates, travel information, number of sources tested, and testing of imported foods. The sources included in the models also differed between the countries. These differences reflect not only availability of data, and thus coverage of national surveillance programmes, but also differences in consumption habits and in the importance of the sources. Cases were attributed to an “unknown” source if they were caused by subtypes not found in the sources considered in the model, or caused by subtypes grouped into “other serotypes”, which the model could not attribute to any of the sources. All models were run in the WinBUGS 1.4 software with five independent Markov chains of 40,000 iterations, each starting with a different set of initial values for the prior distributions. Convergence was monitored using the methods described by Gelman and Rubin (Gelman and Rubin, 1992) and was considered to have occurred when the variance between the different chains was not larger than the variance within each individual chain, and when the chains had reached a stable level.