Treatments and Prevention
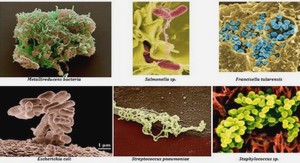
Since HIV was characterized III 1983 and in spite of numerous trials by pharmaceutical companies and academic institutions around the world to develop drugs or vaccines, there is neither an effective HIV vaccine nor a cure for AIDS. However, a variety of treatments are available that can delay progression of the symptoms and improve the quality and length of patients life. In the absence of treatment, almost all infected people develop AIDS. However, a small group of patients called long-term nonprogressors, develop AIDS very slowly or never at aIl in the absence of antiretroviral therapy (ART) over many years of infection (Sheppard et al. 1993; Lisziewicz et al. 1999). It seems that these patients have genetic particularities that significantly prevent the virus from destroying their immune system (Cohen et al. 1998; Kindberg et al. 2006). There are different approaches and strategies toward the treatment or prevention of HIV infection; drug treatments, prevention of mother-to-child transmission, pre-exposure prophylaxis (PrEP), post exposure prophylaxis (PEP), and vaccines. Currently, however, there is no effective vaccine against HIV. HIV is unusual in having a low density of envelope protein spikes on its surface (Fig. 1.3) (Zhu et al. 2006b). Therefore, effective neutralizing antibodies can’t be generated through self-reactive intermediates due to low-density epitope display (Schiller & Chackerian 2014). Moreover, the high error rate ofHIV reverse transcriptase combined with the estimated in vivo HIV-l replication rate often billion new virions each day leads to extraordinary genetic diversity of HIV (see section 1.1.4). This contributes to escape immune pressures and also to the difficulties in producing a vaccine.
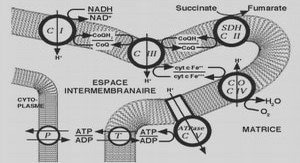
The first approved anti-HIV drug, AZT, was presented on 1988 that targets RT (Young 1988). By using HIV medicines (ART) consistently, progression to AIDS is prevented in most cases. ART helps control the virus so that infected people live longer and healthier and reduce the risk of transmitting HIV to others. The standard treatment, called highly active antiretroviral therapy (HAART) , consists of a combination of antiretroviral drugs against different viral targets. HAAR T prevents drug resistance and increases the chances of survival (Pomerantz & Hom 2003). After viral repli cation is suppressed by HAART for 12 weeks, the number of circulating CD4+ T cells are considerably elevated. Although HAART improves chances of survival by decreasing the HIV -1 burden on the immune system and preventing opportunistic infection, it is expensive (Levy et al. 2006). The UNAIDS Fast-Track strategy (90-90-90), launched in 2014, aims to greatly step up the HIV response in low- and middle-income countries to end the epidemic by 2030.
The strategy calls for 90% of HIV -infected individuals to be diagnosed by 2020, 90% of whom will be on ART and 90% of whom will achieve sustained virologic suppression. The strategy sets targets for prevention, treatment and hum an rights (Jamieson & Kellerman 2016). Another important concem is the appearance of drugresistant strains ofHIV due to the expansion ofHAART (Celum 2011). PrEP is a prevention approach for people who are considered at high risk of HIV infection. It consists in providing them with antiretroviral drugs in order to prevent infection by any possible exposure to the virus (WHO 2011). When taken consistently, PrEP has been shown to reduce the risk of HIV infection in people who are at high risk by up to 95% (Grant et al. 2010). However, PrEP is much less effective if it is not taken consistently. Health care workers are offered post exposure prophylaxis (PEP) ifthey have been exposed with HIV during their works. It may be effective to decrease the risk of infection (Cohen et al. 2005; Smith et al. 2005).
mV-llatency
A successful antiretroviral therapy reduces the HIV load in plasma to undetectable levels but it is not able to eradicate the virus. The mechanism by which HIV -1 persists in the presence of ART is not c1ear yet. The most widely accepted mechanism is that the virus can establish a state of latent infection in CD4+ T cells, in which the provirus is integrated into the host cell genome but is transcriptionally inactivated and thus cannot be targeted by antiretroviral drugs or the immune system (Van Lint et al. 2013). Thus, this type of cells carry a viral reservoir and are responsible for HIV infection being a chronic rather than acute disease. The latent reservoir is now recognized as the major barrier to HIV -1 eradication because it persists ev en in the presence of HAAR T and any treatment interruption results in rapid viral rebound following cellular activation (Jubault et al. 1998; Davey et al. 1999; Richman et al. 2009). The latent form ofHIV -1 infection was first demonstrated in vivo in a small fraction of resting memory CD4+ T cells which were found to harbor the HIV reservoir (Chun et al. 1995).
The frequency ofthese cells is extremely low, typically around 1 per 106 cells (Chun et al. 1997). It was later shown that latency occurs early during acute infection, likely within 10 days of initial infection (Chun et al. 1998). Although more studies revealed that there are several potential cellular and anatomical reservoirs for HIV -1 that may contribute to long-term persistence of the virus, the most pro minent one is CD4+ T cell subsets, primarily resting central memory T cells (TCM) and translational memory T cells (TTM) (Chomont et al. 2009). HIV-l entry in resting T cells may result in the accumulation of non-integrating viral DNA in the nucleus due to a block at reverse transcription, demonstrating that cellular activation is required for efficient infection and subsequently latency (Stevenson et al. 1990; Zack et al. 1990; Descours et al. 2012). Therefore, latently infected resting memory T cells may be generated from antigen-stimulated active T cells infected by HIV and survive long enough to revert back to a resting memory state (half-life of about 44 months) which is then non-permissive for viral gene expression (Pierson et al. 2000; Siliciano et al. 2003; Siliciano & Greene 2011).
Therapeutic approaches to revert the latent state
Several therapeutic approaches, generally termed shock and kill strategy, aim at reactivating proviral expression to revert latency. Patients remain on standard antiretroviral therapy (to block viral spread) while a second drug (shock agent; classes of drugs known as latency-reversing agents (LRAs)) is used to activate latent HIV, followed by the elimination of reactivated reservoirs through either natural means (e.g. immune response) or artificial means (kill agent; e.g. drugs, monoclonal antibodies, etc.) (Hamer 2004). Of particular interest, sorne shock agents are HDAC inhibitors (HDACis) and are the most advanced drugs as HIV antilatency agents in clinical trials (Archin et al. 2012). Combination therapy with valproic, an HDACi, and intensified HAART safely accelerates clearance of HIV from resting CD4+ T cells in vivo (Lehrman et al. 2005). The suberoylanilide hydroxamic acid, SAHA (also known as vorinostat), another HDACi used in this study, has also shown potent activity in reactivating latent HIV (Archin et al. 2009; Contreras et al. 2009). However, a recent study revealed that SAHA increases the susceptibility of uninfected CD4+ T cells to HIV by increasing the kinetics and efficiency of postentry viral events (Lucera et al. 2014).
Moreover, treatment with sorne HDACis including SAHA was found to suppress IFN-y production at early time-points, whereby HDACis suppress the ability of cytotoxic T-Iymphocytes (CTL) to kiIl HIV -infected cells (Jones et al. 2014). Also due to the mutagenic potential of SAHA in in vitro assays, its long-term administration in humans is not allowed (Margolis 2011). Novel HDACis are then needed to consider to reduce toxicity and increase the efficiency. Histone methylation may also reinforce HIV -1 latency. Specific histone methyltransferase inhibitors such as BIX01294 have been reported to reactivate latent HIV -1 with minimal toxicity and causing T cells activation (Imai et al. 2010). Although promoting viral transcription by shock agents results in the reactivation of latent virus, it is not sufficient to eliminate the HIV reservoir. Stimulation of CTLs with HIV -1 specific antigens such as Gag peptides and the cytokine IL-2 prior to virus reactivation in latent CD4+ T cells has led to rapid and effective killing of the infected cells. Therefore, immune-based therapy has been proposed in combination with other shock agents to enhance the clearance of the reactivated reservoir (Shan et al. 2012). AIso, IL-15 has been introduced as shock agent that exposes HIV -Infected resting CD4+ T Cells to recognition by CTLs (Jones et al. 2016).
ACKN »OWLEDGEMENTS |